The BiRT team, based at the Institute of Medical Physics, University of Sydney, is working on methods using Artificial Intelligence (AI) and medical imaging techniques to define the biological distribution of cells in a cancer. Our goal is to use the 3D representation of tumour heterogeneity to determine the optimal distribution of radiation that will effectively treat the cancer whilst minimising harm to surrounding normal tissue. By understanding the Biology of the disease, we can focus our Radiation Treatments to deliver a personalised treatment.
We call this approach Biologically targeted Radiation Therapy, or BiRT.
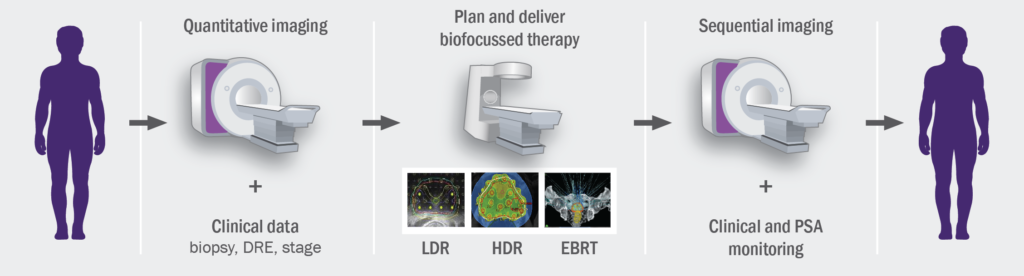
The BiRT team is developing predictive models to extract biological information from advanced imaging methods such as multi-parametric MRI, so that quantitative imaging data can be used to optimise radiotherapy treatment planning. We have traditionally treated tumours as though they were made up of a group of genetically identical cells. However, tumours are made up of different sub-groups – some are more likely to do harm than others. This is called tumour heterogeneity, which is often ignored when we treat patients. This also explains why we see some tumours shrink after treatment, but not completely disappear. In this case, some of the tumour cells have responded well to treatment, but those left behind are resistant to treatment and may start to grow or metastasize after treatment has ended.
Our goal is to use the 3D representation of tumour heterogeneity to determine the optimal distribution of radiation that will effectively treat the cancer whilst minimising harm to surrounding normal tissue. By understanding the Biology of the disease, we can focus our Radiation Treatments to deliver a personalised treatment. Furthermore, response to treatment can be evaluated with frequent repeat imaging so that early intervention can be applied should recurrent disease be detected.
Learn more about BiRT
BiRT Projects