BiRT Team Leader

Professor Annette Haworth
Prof. Haworth is a fully qualified medical physicist with more than 20 years hospital based, clinical medical physics experience. She has held an academic position at the University of Sydney since September 2016.
Prof. Haworth has been involved in cancer research since 1994 when she led the first team in Australia to implant prostates with small radioactive seeds using an ultrasound guidance system. Since treating the first patient with that technique, Prof. Haworth has trained many physicists and clinical teams in this technique. She was awarded a PhD with distinction for work in this area in 2005. She is recognised both nationally and internationally for her expertise in radiation therapy using both radioactive sources (brachytherapy) and external beam radiotherapy, having led several projects that have translated her research into clinical practice.
Prof. Haworth has had a long involvement with the clinical trials group TROG which is Australia and New Zealand’s only clinical trials group dedicated to trials involving radiation therapy. She was the physics representative on the Scientific Committee for 10 years and is now a Life member and a Member of the Board of Directors in recognition of her skills, dedication to clinical trials and recognition as a leader in the field of Medical Physics. TROG provides an ideal platform for reaching out to both the broader national and international clinical community, and patient consumer groups.
In her role as Director of the Institute of Medical Physics at the University of Sydney, Prof. Haworth is the course coordinator for the post-graduate courses in Medical Physics. Through this role she acts as mentor for the next generation of medical physics and is proud to offer a course that reflects the current and future needs of the next generation of medical physicists.
Overview
Our team of physicists, computer scientists, doctors, surgeons and pathologists are working together to devise radiation therapy treatments that are tailored to the specific patient. Unlike other treatments where the same radiation dose is delivered to all patients with the same type of tumour, our goal is to customise the radiation dose to the specific patient, not the specific tumour. We want to deliver just the right amount of radiation to cure each cancer without causing lasting side effects. Our team is working on methods using AI and medical imaging techniques to define the biological distribution of cells in a cancer. We want to design and deliver radiation treatments whereby only the treatment resistant cells get very large doses of radiation, whilst the less aggressive cells get lower doses. This way we can maximise the chances of effectively treating the cancer whilst minimising the radiation dose, and hence harm, to the healthy surrounding tissue.
Our research
The BiRT project received its first grant funding in 2010 with the goal of developing a framework for personalised treatment of prostate cancer incorporating quantitative biologically features derived from multiparametric magnetic resonance imaging (mpMRI). The role of mpMRI was to define the spatial distribution of tumour characteristics to inform a biological model for the purpose of radiation therapy treatment planning. In 2016, an NHMRC grant was awarded to further this work, and in 2019 a SW-TCRC grant was awarded to expand this project across multiple tumour sites. Two of our post-doctoral fellows are independently supported through career / research Fellowship grants and a third member is supported by the Radiation Oncology Network, Westmead Hospital.
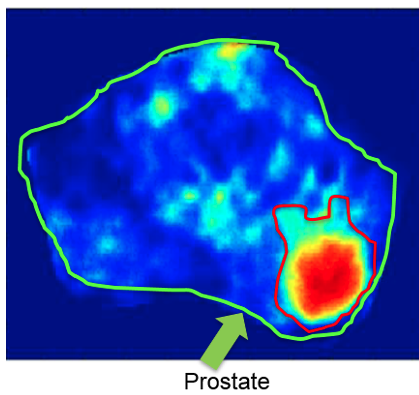
Most of our work so far has been focused on prostate cancer. Our team has applied AI methods and mpMRI to map tumour location and also determine the aggressive nature of the tumour so that we can use mathematical algorithms to precisely calculate the radiation dose that we need to deliver to each part of the prostate. In the image below our computer has produced a heat map that shows we have an aggressive core of tumour shown in red at the centre of the larger tumour area bounded by the red line. Only the red parts of the tumour need very high doses of radiation. This means we can deliver less radiation distant from the central aggressive core. This approach suggests we can provide a treatment with long term survival without damaging the urethra, rectum, bladder and surrounding nerves and hence reducing the risk of side effects from treatment.
Following treatment, we can repeat mpMRI imaging on an annual basis to confirm the treatment has been effective. We predict that using our AI approach we can detect early signs of relapse offering the potential for early salvage therapy. Currently we observe the PSA level in the blood and if it starts to rise we wait a while to see if it is still rising and then we offer treatment, which may be too late for a localized treatment if the disease has already metastasised. We currently have 2 clinical trials testing the feasibility and effectiveness of this approach. (ANZCTR UTN U1111-1221-9589)
Our research work now also includes other tumours including liver, breast and rectal cancer. Regarding liver: some cancers are very difficult to treat if part of the liver is not functioning well, for example due to cirrhosis. We are looking at novel imaging methods that can very carefully and accurately monitor the response to treatment so that we can adjust treatments as they progress so that we do not cause further, unacceptable harm to the tissue surrounding the tumour. In breast, we are looking for special “features” in imaging using Deep Learning methods that can help us predict response to treatment so that patients can avoid surgery that removes the entire breast (mastectomy). In advanced colorectal cancer we are similarly using Deep Learning methods that can help us predict response to treatment so that patients can avoid surgery that removes the entire rectum.
BiRT Projects
BiRT Research Publications
We are currently working with the National Particle Treatment and Research Centre in the development of a business case to bring particle therapy to NSW. The first Australian proton therapy facility will be opened in Adelaide in 2023. Our goal is to bring protons and heavy ions to NSW so that we can treat children and adults with rare and very aggressive tumours more effectively than our current x-ray methods. The BiRT research work is well aligned with these treatments that require precise understanding of the underlying biology of the disease. Our expertise in clinical translation and research work in this area provides us with unique opportunities for leadership in a project that will attract significant national and international interest.
