Advanced validation of mpMRI and PET with pathology
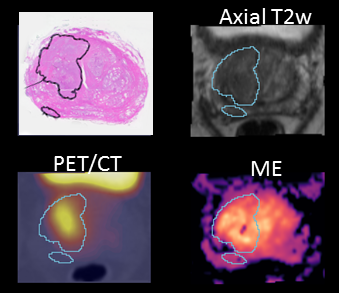
As part of the BiRT project, we have acquired a comprehensive imaging dataset from 70 prostate cancer patients including multiparametric MRI, ex vivo MRI, PET/CT and ground truth histology data. Using our sophisticated co-registration framework, we are conducting advanced correlation analyses using radiomics methods to validate mpMRI and PET with histology. These advanced analyses will provide important supportive information for BiRT treatment planning.
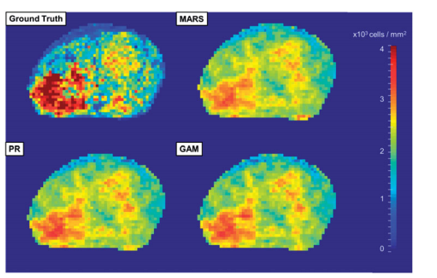
The Prostate Atlas
The BiRT prostate atlas project is aiming to develop a model of the biological properties of prostate cancer. This tool will give us the ability to better understand underlying tumour characteristics. We can use the biological atlas to predict the tumour biology for an individual patient and personalise radiotherapy to deliver more dose to where it is needed, and less to where it isn’t.
Here’s a video for a quick introduction.
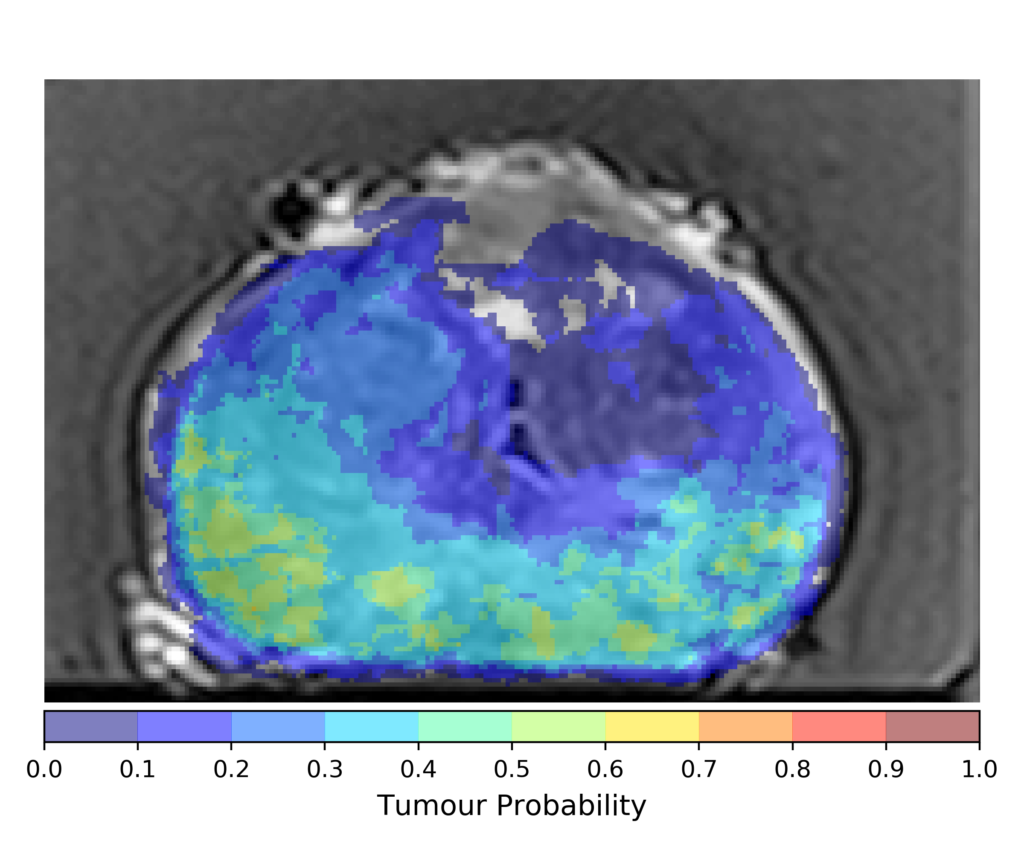
Machine Learning and Radiomics
Machine learning techniques have been used to estimate the tumour location as well as its biological characteristics from the multiparametric MRI data. The intention is to extract patient-specific information from medical imaging (radiomics) which can be used to personalise the radiation therapy treatment. This approach applies a non-uniform dose distribution to the prostate, which can spare healthy tissues while maintaining tumour control.
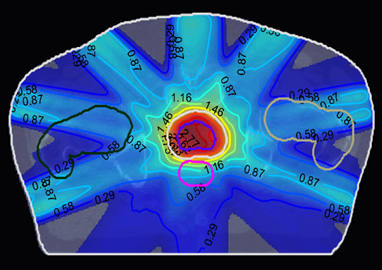
Radiobiology and Optimisation
Our personalised approach with a non-uniform dose distribution has been compared against the conventional treatment planning. The result shows an improved tumour control probability (TCP) while sparing the healthy tissues. The BiRT principles were applied to prostate intensity-modulated radiotherapy (IMRT) to assess the feasibility and dosimetric benefits of the proposed approach compared to uniform-dose planning. The biologally targeted plans demonstrated potential in producing dose distributions with high tumour control and lower rectal and bladder toxicity compared to dose-based planning methods, across several dose fractionation schedules. This is an advance compared with the current non-discriminative approach which delivers a uniform high dose to the entire prostate.

Sequential Imaging (SI-BiRT)
Patient follow-up data has been analysed to track the changes on the multiparametric MRI data. The aim is to identify imaging biomarkers which can predict treatment outcome and patient survival. Imaging biomarkers are characteristic features in the image which can be predictive or prognostic. In this ongoing project, a panel of radiomics features have been computed from the imaging data, which are currently studied over the course of follow-up.
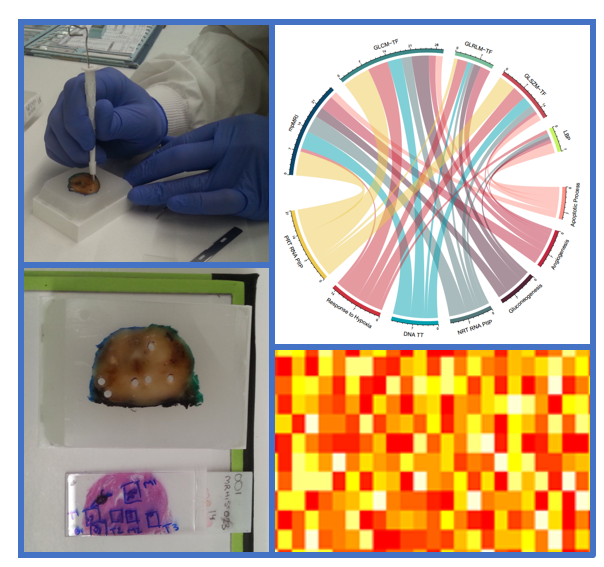
Hypoxia and Radiogenomics
We have designed and performed studies to bridge the gap between the imaging phenotype and the underlying biological genotype. Punch biopsies were taken from the FFPE samples which were sent for transcriptome sequencing. Meanwhile, the corresponding MRI data was analysed by extracting texture features. Weak correlations were found between the imaging features and certain gene expressions. To reduce the false discovery due to the high dimensionality of the genetic data, this study focuses on the hypoxia-related gene set. This ties with the general interest in hypoxia of prostate cancer, which is still currently under-studied.
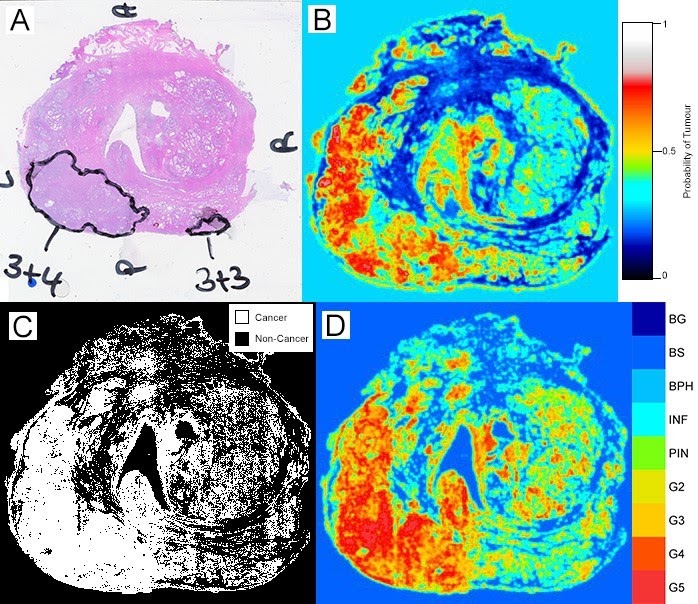
Histopathology Analysis using AI
Manual analysis of histopathology data is labourious, but the information is important to our BiRT framework. One of our project therefore focuses on the use of machine learning and deep learning to automatically predict and grade prostate cancer in histopathology data. Currently, we have are exploring the use of support vector machines and transfer learning methods to develop and refine histopathology prediction models.
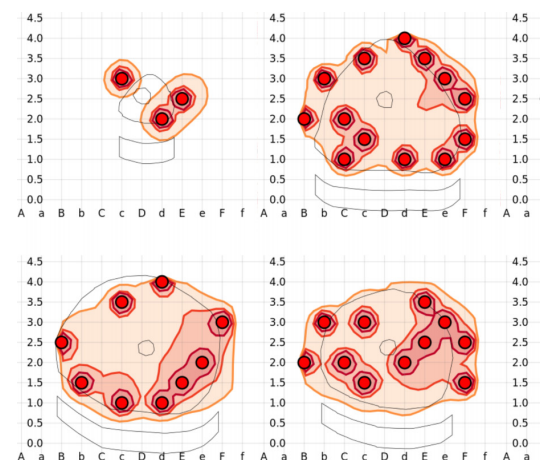
Brachytherapy
Whilst most radiotherapy treatments are delivered using high energy, X-ray producing machines (called linear accelerators, or linacs for short), radiation can also be applied by implanting radioactive sources into the tumour, known as brachytherapy. These radioactive sources may either be implanted permanently or removed after the radiation has been delivered. Because the radioactive source is implanted directly in the tumour, the healthy tissue surrounding the tumour receives very little radiation. The BiRT team have developed dose optimisation methods that determine precisely where the radioactive sources should be implanted in the tumour to deliver the optimal dose of radiation. (Image courtesy: John Betts)
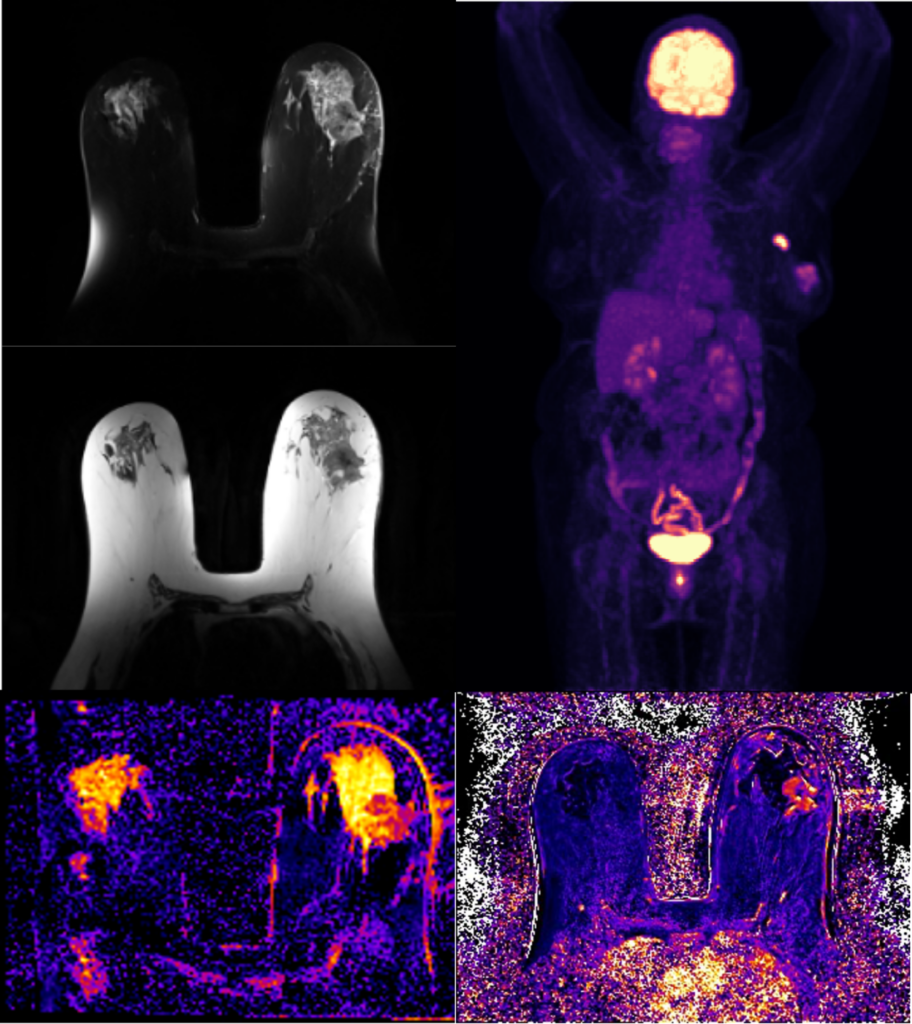
Delta-radiomics for prediction of treatment response in breast cancer
Locally advanced breast cancer is typically treated with primary systemic therapies (PST) to render the tumour operable. Response to PST is traditionally measured using mammograms and ultrasound (US), which often underestimate tumour volume and extent of disease. The PET-LABRADOR clinical trial was designed to test the hypothesis that breast MRI and PET-CT imaging can accurately predict operability after PST, without compromising local control or disease-free survival. Recent studies highlight the potential of multi-parametric breast MRI and PET-CT based radiomics for accurate assessment and prediction of response of breast cancer to PST. In this work, we propose to examine the feasibility of radiomics analysis of longitudinal breast MRI acquired in the PET-LABRADOR clinical trial and evaluate changes in radiomics features pre, during and post-PST.
Personalisation of liver stereotactic body radiation therapy using MRI
Stereotactic body radiation therapy (SBRT) is a relatively new treatment option for primary liver cancer (hepatocellular carcinoma, HCC) showing incredibly promising survival outcomes, as it enables high doses to be delivered very precisely. Patients with good liver function (measured using blood tests) are candidates for this treatment. However, a significant proportion of HCC patients have impaired liver function and are currently denied SBRT, or offered SBRT with significantly reduced radiation dose in order to preserve liver function. The low doses are sufficient to only slow disease progression,
In this project, magnetic resonance imaging (MRI) is used to create images of the liver that show regions of high and low function. A methodology for personalised SBRT will be developed, where radiation beams are directed at the tumour to avoid intersection with high functioning liver, thus preserving the patient’s overall liver function while enabling high radiation doses to be given to the tumour. This novel treatment approach will open up a treatment pathway and offer hope to patients previously given a dismal prognosis.
